PUBLIC HEALTH – Osteoarthritis (OA) is one of the most common forms of arthritis, affecting millions of people worldwide. It’s a chronic condition that leads to the breakdown of joint cartilage, causing pain, stiffness, and decreased mobility. If you’re dealing with osteoarthritis, you’re not alone. Whether it’s affecting your knees, hips, hands, or spine, OA can significantly impact your daily life.
In this comprehensive guide, we’ll dive into what osteoarthritis is, its causes, symptoms, and the most effective ways to manage and treat it. We’ll also explore lifestyle changes, exercise tips, and medical treatments that can help you live better with this condition.
What Is Osteoarthritis?
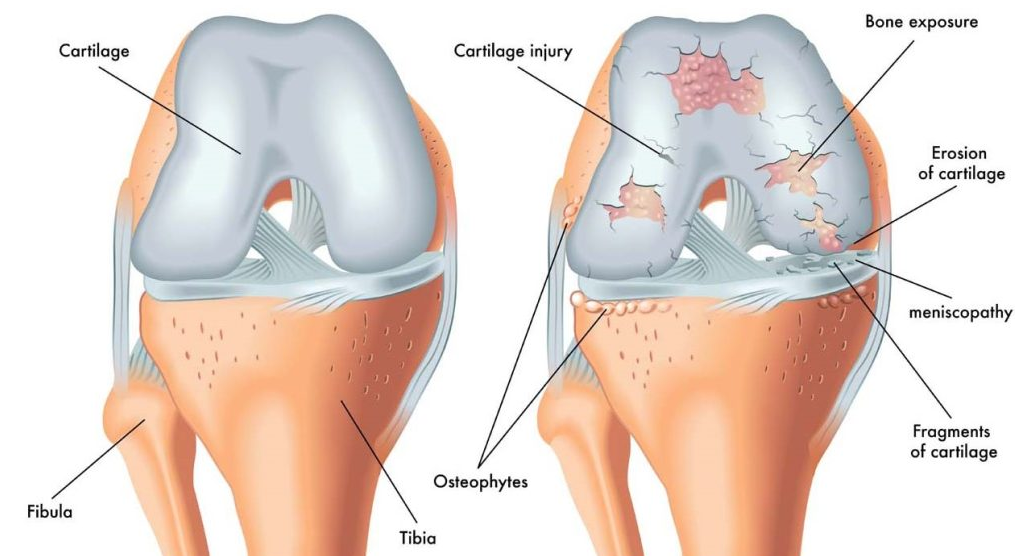
Osteoarthritis is a degenerative joint disease that affects the cartilage in your joints. Cartilage is the smooth tissue that cushions the ends of your bones and allows for easy movement. When this cartilage breaks down, bones can rub together, causing pain, swelling, and stiffness. Over time, the condition can lead to joint deformity and loss of mobility.
Although OA can occur in any joint, it most commonly affects weight-bearing joints such as the knees, hips, and spine. It can also impact the small joints in your hands and fingers.
Causes of Osteoarthritis
The exact cause of osteoarthritis is still not fully understood, but several factors can contribute to its development:
- Aging: As we age, the cartilage in our joints naturally starts to break down. This is why OA is more common in older adults.
- Joint Injury: Previous injuries or trauma to a joint, such as fractures or ligament tears, can increase the likelihood of developing OA.
- Genetics: Family history plays a role. If your parents or siblings have OA, you may be at higher risk of developing it.
- Obesity: Extra body weight puts additional strain on weight-bearing joints like the knees, increasing the risk of developing OA.
- Overuse: Repetitive motions or overuse of certain joints in daily activities or occupations can wear down cartilage over time.
Risk Factors for Osteoarthritis
While osteoarthritis can affect anyone, certain factors can increase your risk:
- Age: OA typically develops after the age of 40, and the risk increases with age.
- Gender: Women are more likely to develop OA than men, especially after menopause.
- Family History: If osteoarthritis runs in your family, you may be more predisposed to it.
- Joint Injuries: Injuries from sports, accidents, or surgery can increase the risk of developing OA in the affected joint.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis can vary depending on the severity of the condition and the joints involved. Here are some of the most common signs:
1. Joint Pain
Pain is the hallmark symptom of osteoarthritis. It typically worsens after physical activity and improves with rest. The pain may start as mild discomfort but can become more intense as the cartilage continues to break down.
2. Stiffness
Stiffness is common, particularly after periods of inactivity, such as when you wake up in the morning or after sitting for a long time. It may take time for the joint to loosen up, especially if the condition is advanced.
3. Swelling
As the cartilage wears away, the joint may become inflamed, leading to swelling. This is most noticeable after extended use of the affected joint.
4. Decreased Range of Motion
As the joint becomes more damaged, it can become harder to move. You may notice that bending, twisting, or performing other motions becomes more difficult.
5. Crunching or Grating Sensation
You may feel or hear a sensation known as crepitus, which occurs when the rough surfaces of the bones rub together. This is common in joints like the knees and hips.
6. Joint Deformities
In more severe cases of osteoarthritis, the joint may become misshapen or enlarged. This is due to the growth of bone spurs, which can form around the edges of the affected joint.
Managing Osteoarthritis: Treatment and Lifestyle Changes
While there is no cure for osteoarthritis, there are several treatment options available to manage symptoms and improve your quality of life. The goal of treatment is to reduce pain, improve joint function, and slow the progression of the disease.
1. Medications
Medications can help manage the pain and inflammation associated with osteoarthritis. Common options include:
- Pain relievers: Over-the-counter (OTC) pain medications, such as acetaminophen (Tylenol), can help manage mild pain. For more severe pain, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen may be recommended.
- Topical treatments: Creams and gels containing NSAIDs can be applied directly to the skin over the affected joint to reduce pain and inflammation.
- Corticosteroid Injections: These injections can provide temporary relief by reducing inflammation and pain in the affected joint.
2. Physical Therapy and Exercise
Regular exercise and physical therapy can play a key role in managing osteoarthritis symptoms. A tailored exercise program can help:
- Improve joint flexibility and strength
- Reduce pain and stiffness
- Improve balance and coordination
- Prevent further joint damage
Low-impact exercises like swimming, cycling, or walking are ideal for people with OA, as they put less stress on the joints while still promoting movement and muscle strength. A physical therapist can guide you through exercises that target specific areas of concern.
3. Weight Management
If you’re overweight, losing weight can significantly reduce the pressure on weight-bearing joints, such as the knees and hips. Even a modest amount of weight loss can reduce the symptoms of osteoarthritis and slow its progression.
4. Joint Protection
Using supportive devices like knee braces or special insoles can help protect your joints during daily activities. Additionally, modifying your environment to minimize stress on your joints can prevent further damage. This might include using ergonomic furniture or assistive devices.
5. Alternative Therapies
Some individuals find relief from osteoarthritis symptoms through complementary therapies, such as:
- Acupuncture: This traditional Chinese practice may help alleviate pain and improve mobility.
- Massage therapy: Regular massage can reduce muscle tension and improve joint function.
- Supplements: Supplements like glucosamine, chondroitin, and turmeric may help reduce inflammation and improve joint health, though evidence on their effectiveness varies.
6. Surgical Options
In severe cases of osteoarthritis, when other treatments no longer provide relief, surgery may be necessary. Surgical options include:
- Arthroscopy: A minimally invasive procedure where a small camera is used to remove damaged tissue or clean out the joint.
- Joint Replacement: If the joint is severely damaged, joint replacement surgery (such as knee or hip replacement) may be recommended. This procedure involves removing the damaged joint and replacing it with an artificial one.
Living with Osteoarthritis
While osteoarthritis is a chronic condition, there are many ways to maintain an active and fulfilling life. Managing OA requires a combination of medical treatment, lifestyle adjustments, and self-care.
Here are some additional tips for living with osteoarthritis:
- Stay Active: Regular, gentle exercise can help keep your joints flexible and reduce stiffness. Consult with a doctor or physical therapist to find an exercise program that’s safe for you.
- Mind Your Posture: Maintaining proper posture while sitting, standing, and walking can help reduce stress on your joints.
- Manage Stress: Stress can exacerbate symptoms of osteoarthritis. Practices like meditation, deep breathing, and yoga can help manage stress and improve your overall well-being.
Conclusion
Dealing with osteoarthritis can be challenging, but it’s important to remember that you have options for managing the condition. By staying informed about the causes, symptoms, and treatment options, you can take proactive steps to reduce pain and improve your quality of life. With the right combination of medical care, lifestyle changes, and self-care strategies, you can continue to lead an active, fulfilling life despite the challenges of OA.
If you’re experiencing symptoms of osteoarthritis, it’s always a good idea to consult with a healthcare provider. They can help you develop a personalized treatment plan to manage your symptoms and improve your joint health.